November 11, 2020
Healthcare is hard. A colleague of mine succinctly describes with two words our current problem in our care delivery system: overwhelming complexity.
If you work in or around healthcare, you know this to be true. Unfortunately, it is not getting any better either. Consider what we are seeing in the headlines over the last 10 months related to COVID-19. The virus completely overwhelmed our health systems in short order, because of the adversarial nature of interoperability that exists in health and public health in the United States.
We have struggled greatly to manage the spread of the virus and treat the patients flooding into our care delivery system in 2020, because care components operate independently of one another. The COVID-19 struggle has exposed many deficiencies of technology we have invested billions in annually–all in an effort to better treat and manage disease in America.
Why haven’t we treated and managed this crisis better?
It is easy to point fingers at the leadership at different levels of our public and private health systems in how they have managed this pandemic. Yet, there was a greater fundamental issue at play long before we found our country in this current crisis.
The information needed to help predict and prevent the spread of COVID-19 in our communities and understand the capacity of our local hospitals and health systems to treat patients is locked away inside medical records and lab information systems.
We have built a sophisticated system over the last decade of capturing information as we have transitioned from paper-based records to electronic medical records and lab information systems.
The cost of care continues to grow out of control.
As a patient, we should expect services that cater to our individual needs. Instead, we pay more than almost any other country in the world for a system that operates under a one-size-fits-all, trial-and-error model that wastes $765 billion annually. This care is riddled with missed diagnoses, protracted illnesses, and premature death that is preventable given all the information available.
The human toll is even more devastating. More than 128,000 people in the U.S. die each year from simply taking their medications as prescribed—four times the number of people killed by prescription painkillers and heroin combined.
Precision medicine holds promise as the solution to healthcare’s fundamental flaws.
With a single lab test, physicians have information on a patient’s genetic markers, which they can use to determine which treatments will work best and carry the fewest risks for that individual. Yet adoption of precision health remains limited to very narrow patient cohorts like oncology and cardiology. Why is that?
The blame for the lack of adoption of precision health—and healthcare’s flaws in general—is multifaceted. The information clinicians need to deliver personalized, precise care is locked away in disconnected databases, buried in medical journals, and isolated in multiple patient data silos.
Plus, broken incentives continue rewarding quantity over quality, as evidenced by the billions of dollars in government subsidies and incentives targeting broad implementation of electronic health record (EHR) systems that nonetheless failed to deliver access to meaningful clinical insights. We need precision health.
What is precision health?
Precision health as defined by UCLA Health “takes into account differences in people’s genes, environments, and lifestyles and formulates treatment and prevention strategies based on patients’ unique backgrounds and conditions.”.
We are all unique yet our healthcare system is designed to treat everyone the same. This one-size-fits-all model can have adverse consequences for your health if you are not the average patient who responds to a particular treatment or prescription as expected.
There is a reason pharmaceutical companies and retail stores provide a laundry list of side-effects when you fill a prescription or see a commercial about a drug. Our bodies respond differently because we are not all average.
UCLA Health further defines the goals and benefits of precision health care tailored to both providers and patients as giving “the medical team the tools to better understand how complex the human body is. Precision health will help us to keep you healthy. If you do get sick, precision health will help us understand which treatments work best with the fewest side effects.”
Keeping patients from getting sick has additional benefits. It can reduce the burden on our care providers who are suffering from staggering levels of burnout. It can lower the costs of care for patients by ensuring they are on the right treatments the first time. Precision health improves the quality of care for everyone involved.
We need to unlock the full value of precision health if we have any hope of reducing variations in care, addressing health disparities, and lowering and controlling growing costs to deliver quality care.
The CDC highlights the value of precision health in not only our ability to diagnose and treat patients, but also this approach to care “can better predict, prevent, treat, and manage disease.”
Everyone wants to treat and manage the diseases impacting patients that are needing sick care in our delivery system. If we can prevent and predict it before they get sick, that is infinitely better. What will it take to get there with healthcare?
Critical Insights, Analytics, and Solutions for Precision Health
Over 2.3 trillion gigabytes of data are generated every year in healthcare. Equal to:
- 1.2x the amount of currency in circulation in the United States
- 1,000x the amount of heartbeats the average human will have in their lifetime
- Over 20x the amount of people that have ever existed on earth
- 20x the amount of stars in the milky way galaxy
- The amount of steps it would take to walk around the world 35,000 times
- 760 times the amount of base pairs in the human genome
All the data is almost useless without a method to ingest, organize, and normalize it into actionable information that is meaningful for providers and patients. Healthcare professionals require streamlined insights to break through the noise in each 7-minute patient visit.
Precision Health is one of the many silver bullets that has the potential to cure what ails our current U.S. health systems.
Precision Health is powered by more and more data
We have networks that provide our news and entertainment that leverage our interests to suggest information and programming we would find valuable–saving us time and not wasting money on things we would not. We have complex networks that tie together our social and work relationships. Without networks of independent banks working together, we all might be socially distancing at our local branch with masks on trying to perform financial transactions.
Healthcare is the last industry to embrace digital transformation to improve the lives of the people who depend on it and those professionals who work inside our care delivery system. We are seeing huge strides in financial technology that enable safety and security for our financial assets, but not in healthcare for our physical and mental assets.
Why can’t we have secure networks that work together in healthcare?
We can.
The rapid advances in secure cloud technologies powering machine learning, artificial intelligence, and big data in financial services, is available and emerging in precision health and healthcare.
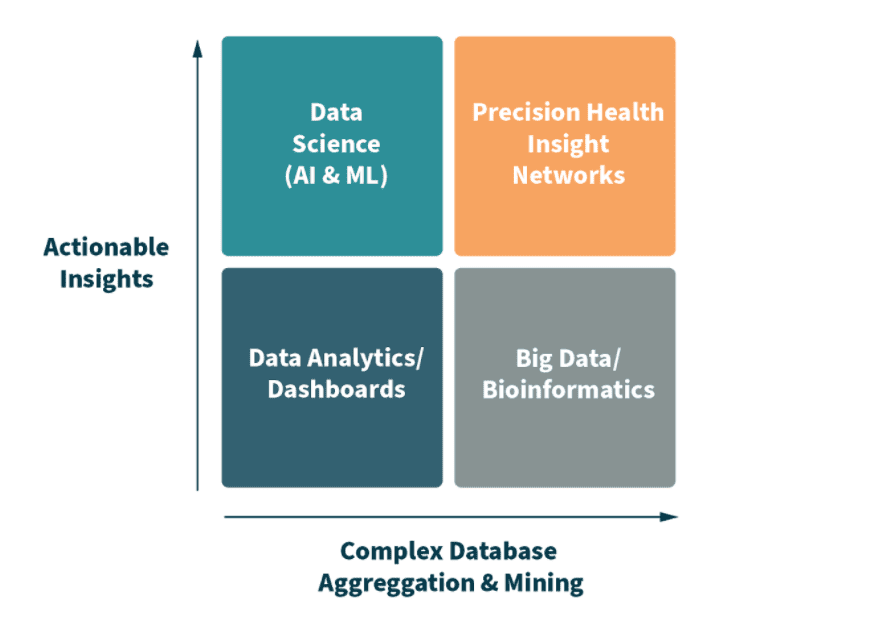
A new category of Precision Health Insight Networks (PHINs) is making this possible for organizations of all sizes in healthcare who are responsible for managing complex patient information securely across networks. These PHINs provide critical insights, analytics, and solutions for precision health with ever-faster time to value.
The beauty of PHINs is they take the stress of wasteful practices out of the system and off the providers who are critical to help usher in this new era of personalized, high-value care everyone can benefit from and embrace—profitably improving patients’ lives through value-based care by identifying and connecting data to the delivery of high-value care.
We have all heard the stories of systems that have invested in data lakes and enterprise data warehouses that have not produced the meaningful and actionable insights promised. Can we all agree that most health systems, providers, and payers simply lack the expertise to securely ingest, organize, and normalize new and expanding data sets in real-time to drive better decision making and improve health outcomes? The cost and effort to maintain the data is growing out of control.
It is incredibly discouraging for our healthcare system to have so little to show after gathering trillions of gigabytes of patient data without usable and meaningful insights.
We’re asking our caregivers to perform an impossible task in our data-rich world. Without the insights provided by precision health, having all of the practice-changing evidence and data sets in the world becomes futile–leaving administrators frustrated and care providers exhausted trying to keep up with complex volume-based models to remain profitable.
New insight networks for precision health solve these complex problems by transforming live data into valuable and actionable healthcare insights much like ATMs did in banking to give you valuable information for your financial assets. PHINs are helping patients and families make it out of the $17 billion healthcare delivery system unscathed by avoiding costly and harmful adverse events.
Experts in Precision Health Insight Networks (PHINs) deliver on precision testing and prescribing for mass personalization that the old-school, volume-based, fee-for-service care models will never achieve.
There simply is no room for these status quo models that deliver ineffective, harmful trial-and-error and costly, one-size-fits-all care that varies wildly from facility to facility.
Now is the time to invest in Precision Health Insight Networks for high-value care. They deliver insights our healthcare leaders and providers can take action on with precision–the right patients, right tests, and right prescriptions. All right now.
These advances in healthcare from PHINs are occurring at the intersection of Digital Transformation, Personalized Medicine, and Population Health today.
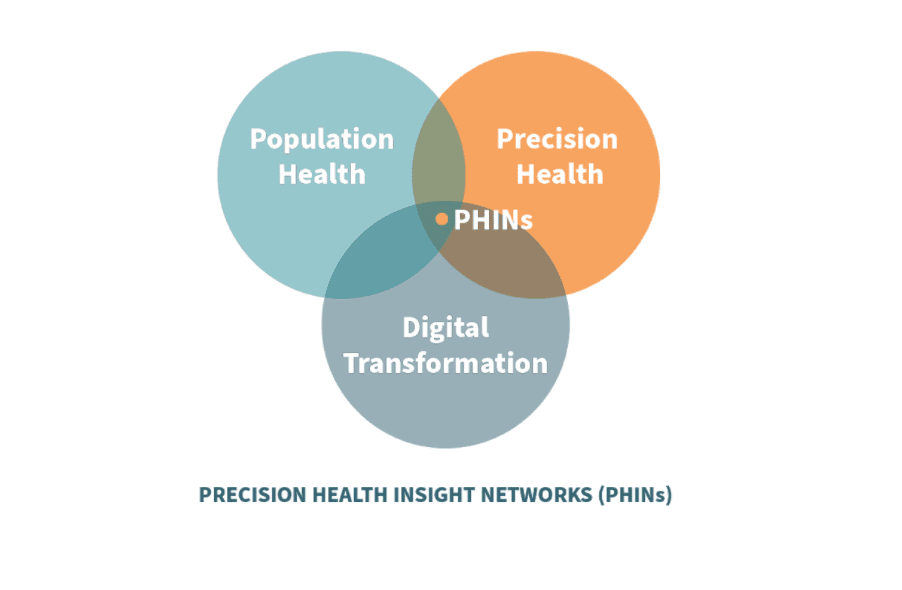
This emerging category of solutions holds tremendous promise to deliver countless breakthroughs that will forever change the way healthcare is delivered, saving millions of lives and billions of dollars.
hc1 powers Precision Health Insight Networks (PHINs)
The hc1 Platform™ is crafted to address the problems with precision health today. The Platform is purpose-built to ingest, normalize, and organize disparate healthcare data at scale; infinitely expandable, immediately accessible, ultra-high availability on the AWS cloud stack. We are the company behind the emerging category PHINs, a topic we will explore in-depth during the Precision Health Virtual Summit with Becker’s and our partners AWS and Quest on November 16-17.
PHINs in action
Everyone knows what happened in the United States during March with COVID-19. All businesses were impacted by the simultaneous national shutdown. A number of businesses decided to furlough employees immediately and wait it out. Others went into action to help. Our CEO Brad Bostic chose to make a difference–by utilizing our technology stack and our lab relationships to help flatten the curve. Within weeks, we had formed a coalition of lab and technology partners, including AWS, to deliver a lab testing dashboard to aid in the fight against the spread.
On April 3, CV19Dashboard.org was made available to frontline workers in healthcare and government with data from over 20,000 lab ordering locations. At the time, much of the data was locked away in case reports that came in as much as 8-14 days in arrears and riddled with errors. Our anonymized dashboard was near-real time with lab results directly from the sources of testing activity. It evolved to provide a real-time Local Risk Index (LRI) that showed leaders where hotspots of virus activity were trending around the US and in local communities. We even built a special version of the LRI county map for Dr. Scott Gottlieb and AEI.org that has had over 100K users since May 1. The hc1 team won awards and recognition for our response to the global pandemic. This coordination and collaboration across labs does not happen without PHINs built on top of outbreak signal solutions powered by AWS. We accomplished in weeks what would have taken others months, if not years, to pull together.
Other solutions were spawned from this insight network solution for COVID-19. A great example is our solution for the state of Arizona with our partner Sonora Quest for their most vulnerable populations in Long-Term Care (LTC) facilities. It was a solution that provided a command center for employees and patients to monitor testing and the spread of the novel coronavirus. Arizona was lauded as a model state for how they addressed the crisis around testing and overcame issues related to data reporting. Our team helped make that happen.
Employers looking to get back into the office or back to campus, now have hc1 Workforce Advisor™ as well, to help them manage through this ongoing pandemic. Like the LTC solution, we have partnered with organizations in lab testing, as well as contact tracing app providers, to integrate our lab testing data, command center, and local risk insights for a full suite employer solution to help employees return with confidence.
Is your organization ready to deliver safe, effective, affordable, and personalized care?
Start by connecting data to delivery with better health outcomes.