October 6, 2022
Changes in seasons often accompany changes in diet, environment and behavior. Such changes can have a cascading effect on health, particularly for people who take prescription medication. Precision prescribing recognizes that every person has a unique combination of genetic, environmental and behavioral factors that will determine how specific medications will work for them.
The term pharmacokinetics describes how drugs move through the body—how they are absorbed, metabolized and eliminated. Pharmacodynamics describes how the drug affects the body. Food-drug interactions are how foods change a drug’s pharmacokinetics and pharmacodynamics. These changes can reduce the medication’s effectiveness or lead to adverse events. The impact of these changes can be difficult to predict because of the many factors involved: how much time elapses between eating and taking medication, the nutritional content of the food, and the amount of food eaten. Age, sex and genetics also affect how a person metabolizes food and medication.
From Pumpkin Spice Lattes and Oktoberfest Märzens to Halloween candy and Thanksgiving dishes, favorite fall foods interact with drugs in different ways:
- Licorice. Before breaking into bags of black licorice this Halloween, you may want to check with your doctor, particularly if you are pregnant or older than 40. Commonly used in herbal remedies as well as candy, licorice contains glycyrrhizin, which can lower potassium. Licorice also can raise cortisol levels. These physiological effects mean that licorice doesn’t mix well with medications for high blood pressure or cardiovascular diseases, such as ACE inhibitors or diuretics. Combining such medication and licorice can lead to irregular heart rhythms.
- Grapefruit. Ruby Red grapefruit season starts in November, and this fruit’s sour kick can be just the ticket when your body needs a vitamin C boost. Yet grapefruit also blocks the CYP3A4 enzyme from metabolizing drugs in the small intestine, causing too much of the drug to be in your body. The affected drugs include some statins, some high blood pressure medication, some anti-anxiety drugs, and some corticosteroids. With some antihistamines, grapefruit prevents absorption of the drug, thus lowering the drug’s effectiveness. Grapefruit interactions are typically highlighted on a prescription’s warning label or the box containing over-the-counter medications.
- Cruciferous vegetables: Thanksgiving feasts have moved beyond green bean casserole to make room for roasted Brussels sprouts and mashed cauliflower, and rightly so. These vegetables from the Brassica botanical family are low in calories, high in fiber, and packed with nutrients, such as Vitamin K. What makes them different from other vegetables is that they contain glucosinolates, compounds that show promise in reducing cancer and cardiovascular disease risk and are the cause of their pungent odor and somewhat bitter taste.
These typically beneficial qualities can work against specific medications, however. Warfarin is a blood thinner used to prevent blood clots; whereas, Vitamin K helps make blood clotting proteins. Drastically increasing your intake of, say, kale chips or green smoothies could interfere with warfarin’s effectiveness. Cruciferous vegetables also increase the activity of the CYP1A2 enzyme, an enzyme involved in drug metabolism. As more drugs are developed that are metabolized via this enzyme, more research will be needed to determine how diets high in cruciferous vegetables might affect the effectiveness of those drugs.
- Aged cheeses and meat. Charcuterie boards are not your friend if you take any of the class of drugs known as monoamine oxidase inhibitors (MAOI). MAOIs are prescribed to treat depression and Parkinson’s disease. As the name suggests, they block monoamine oxidase, an enzyme that breaks down tyramine. Our bodies use tyramine to control blood pressure, and foods such as cheddar cheese, salami and pickles are full of it. If you are taking medication that prevents tyramine from being broken down while ingesting more tyramine, you are likely to end up with too much tyramine, and too much tyramine can cause dangerous blood pressure spikes.
- Beer, wine and liquor. Alcohol is a drug that depresses the central nervous system and can damage the liver. These effects can be increased to dangerous levels when alcohol is combined with medications that have similar effects, such as sedatives and pain relievers. For example, you may become extremely drowsy if you drink alcohol while taking medication to deal with autumn ragweed allergies. Another bad combination is alcohol and acetaminophen, which are both metabolized by the CYP2E1 enzyme and together can lead to liver toxicity.
- Coffee. As the weather gets chillier and the days get shorter, you might pour yourself multiple mugs of coffee to stay warm and awake. Coffee contains caffeine, a stimulant, which gives coffee its bitter taste and has many different pharmacokinetic interactions with prescription drugs. Coffee interferes with drug absorption by changing stomach acid levels, for example, and interferes with drug excretion by increasing urine volume.
Food-drug interactions are one of many patient data points providers have to take into account to create effective treatment plans. Patients will try to make themselves feel better before they ever set foot in a doctor’s office, so patient encounters should include questions about over-the-counter medications, herbal supplements, and diet changes in addition to medical history and current symptoms.
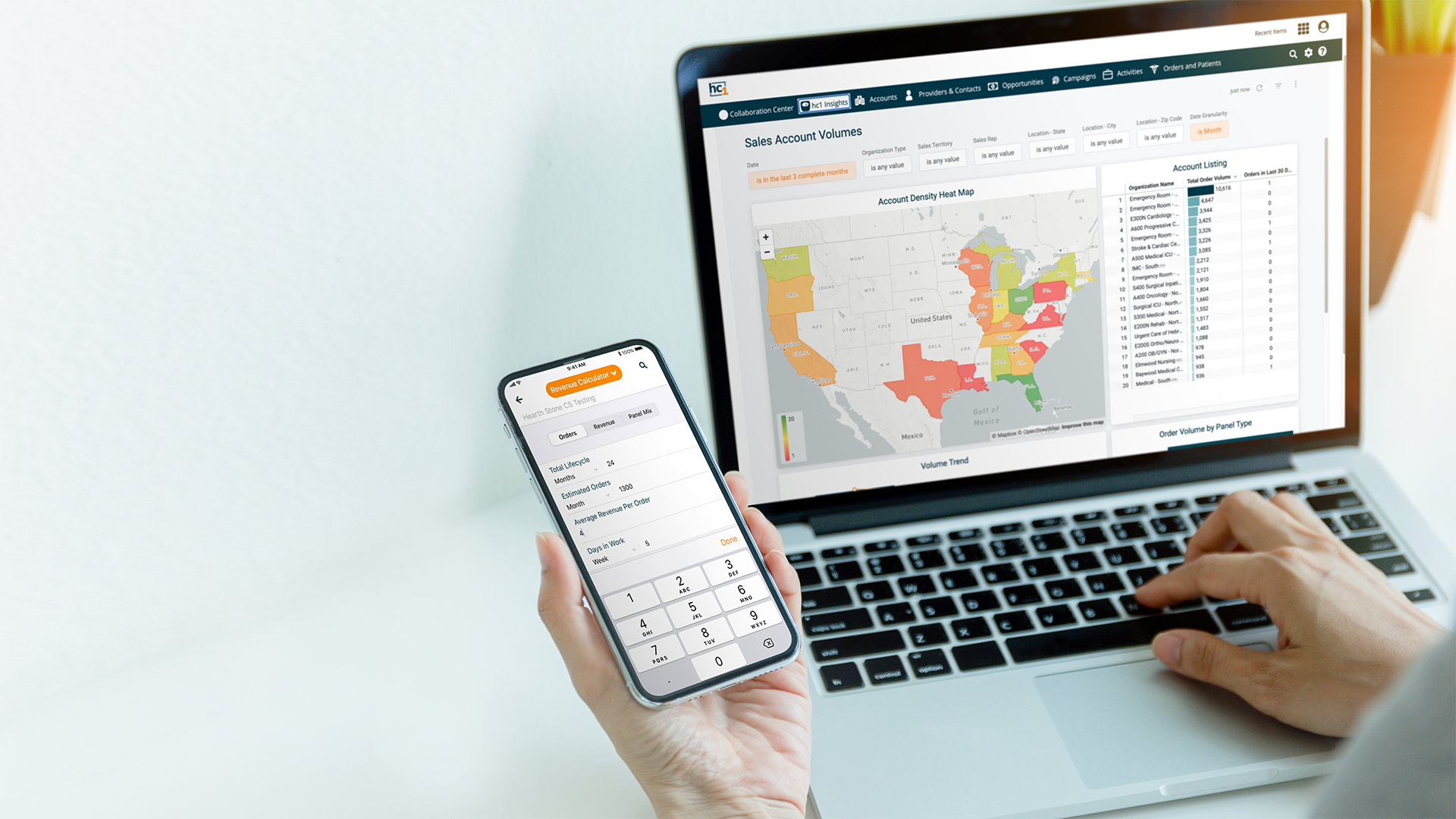
To learn how hc1 can help your healthcare organization ensure that patients get the right tests and the right prescriptions no matter the season, request a demo!