December 6, 2023
Laboratories and health systems track many aspects of their processes and business performance using data such as quality metrics, key performance indicators, test utilization, and individual performance. These measures are commonly presented in an analytic fashion, where data is aggregated over time and presented in a useful way (inclusive of comparison against historical performance). It’s fairly easy to look at a single entity and state “Yes, it’s going well” or “No, this requires intervention” when comparing it to a predetermined expectation or historical data. But how does an individual’s data or independent data point transition into larger perspectives like a department, specialty, hospital, or health system? And how do you know if your lab is the best in the business or has room for improvement? That’s where benchmarking comes into play.
What is Benchmarking?
Benchmarking has been a buzzword in laboratories and health care overall for a while. People hear it and nod enthusiastically, exclaiming, “YES! We want to do that, too!” As is typical with buzzwords, they often mean different things to different audiences, making it difficult to determine if a conversation around benchmarking as a construct is, at its core, the same among participants. For the purposes of this article, the definition of benchmarking will be to evaluate (something) against specific criteria that have been vetted, documented, and measured by an organization and the outcome(s) compared to an organization that is considered ‘the best in the business.’
Let’s clarify that definition a little further. ‘Vetted’ relates to the (something) that is being carefully examined, has value, and is specifically defined. “Documented” relates to why the benchmark of the (something) is important and how it was benchmarked. “Measured” refers to how the benchmark is assessed or valued in support of other entities comparing their data to it.
How do benchmarking and common operational metrics differ?
Benchmarking differs from common operational metrics in that quality metrics or key performance indicators are measured against a predefined lab or facility expectation (which could be an agreed-to standard or be defined by a service level/interdepartmental service agreement). These thresholds may vary across labs within a health network due to department structure (STAT lab in the ED vs. ED work sent to the main lab), facility type (critical access hospital vs. academic medical center), or testing services provided (performed in-house or sent to another facility in the health network). Whether the predefined expectation is “the best in the business” instead of “acceptable” is not considered.
Another difference between benchmarking and operational metrics is that operational metrics are simply a comparison to answer a straightforward question: are we meeting (or exceeding) an expectation or not? It has no insight into “what the best case scenario is and how we evolve to perform in the best way possible.” Done well, that is what benchmarking accomplishes.
Benchmarking takes the concept of operational metrics further, looking at the “best of the best” – where exceptional excellence exists in a comparable environment – moving into the territory of identifying areas of improvement, implementing a plan to support improvement, and continuously analyzing the outcomes throughout the process. (So it’s similar to developing quality indicators to measure process improvement, but often the scope is different and there may be no specific declaration of ‘complete’.)
Are quality metrics the same as benchmarking?
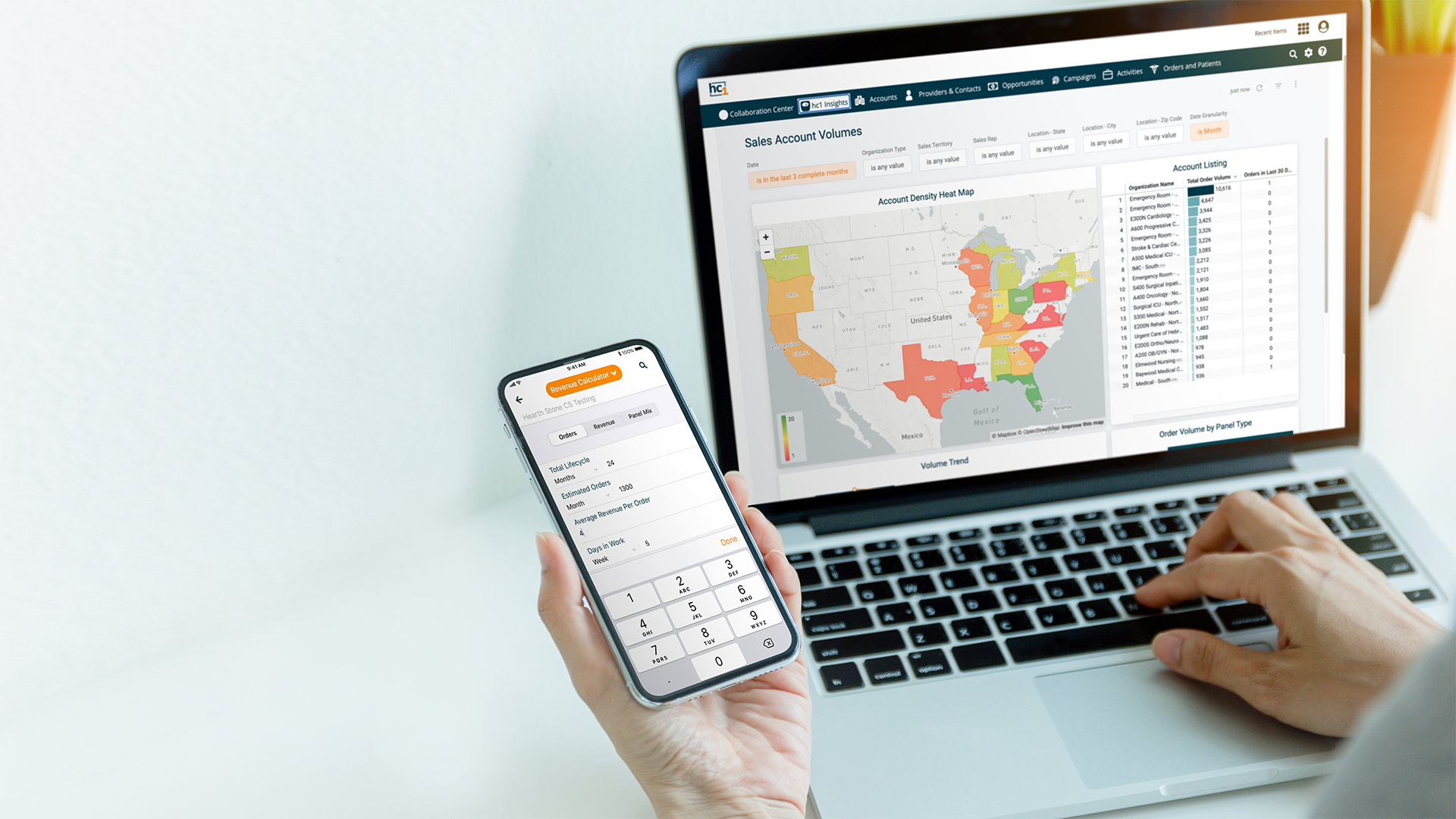
Quality metrics to analyze performance-related analytics are a simpler concept to benchmarking and systems, such as hc1 Performance Analytics and PrecisionDx (PDx) Advisor, support those needs very well. Analytics do not require the depth that benchmarking requires, but they may be a component of the benchmarking process. Understanding how your organization (lab, hospital, etc.) performs is a first step in preparing to benchmark data internally (within your own health network or system), and understanding your internal benchmarking will feed external benchmarking initiatives (anonymous comparison of your benchmarks to a valid, “the best of the best” center of excellence, along with similar organizations who are comparing to the same benchmark).
How can a lab get started with benchmarking?
With benchmarking being a continuous process of comparison of your organization against “the gold standard,” opportunities for improvement often require a committee-type structure to enable learning and adopting best practices learned from the “best of the best” organizations. Benchmarking may be a logical ‘next step’ from a lab stewardship perspective, where the lab already has an understanding of related processes and implemented stewardship-related changes to support best ordering and testing practices within their health system.
Click here to learn more about strengthening or starting a Lab Stewardship program.